Periodontal Disease
Bleeding and swollen gums are early signs that your gums are infected with microbes. If nothing is done in this case, the disease can spread and destroy the structures that provide support to your teeth in your jawbone. In the end, your teeth can turn out to be loose and must be removed to prevent further damage.

Talk to a Dentist Now!
“Perio” signifies around, and “dental” means the teeth. Periodontal diseases are defects of the structure around the teeth, which comprise the gums, periodontal pocket and alveolar bone in the early phase of periodontal disease. This causes gingivitis, which is known as the infection of gums, and it also gives rise to severe types of illness.
What is Periodontal Disease?

“Perio” signifies around, and “dental” means the teeth. Periodontal diseases are defects of the structure around the teeth, which comprise the gums, periodontal pocket and alveolar bone in the early phase of periodontal disease. This causes gingivitis, which is known as the infection of gums, and it also gives rise to severe types of illness.
Periodontal disease is happened due to bacteria in dental plaque, the clingy substance that structures on your teeth two or three hours after you have brushed.
Strikingly, it is your body’s reaction to the bacterial infection that causes the vast majority of the issues. With an end goal to wipe out the bacteria, the cells of your resistant framework discharge substances that cause destruction and inflammation of the gums, alveolar bone or periodontal ligament.
This prompts swollen, bleeding gums, indications of gingivitis (the most punctual phase of periodontal disease), and extricating of the teeth, an indication of serious periodontitis (the propelled phase of disease).
For a long time, researchers have been attempting to make sense of what causes periodontal disease. It is presently very much acknowledged that different sorts of microorganisms in dental plaque are hazardous.
Scientists additionally are becoming familiar with how an infection in your gums can influence your general wellbeing.
Lately, gum illness has been connected to various other medical issues. This is another and energizing territory of research, however, it stays skeptical. Studies have delivered fluctuating answers about the degree of the association between gum sickness and other medical issues, and more research is required.
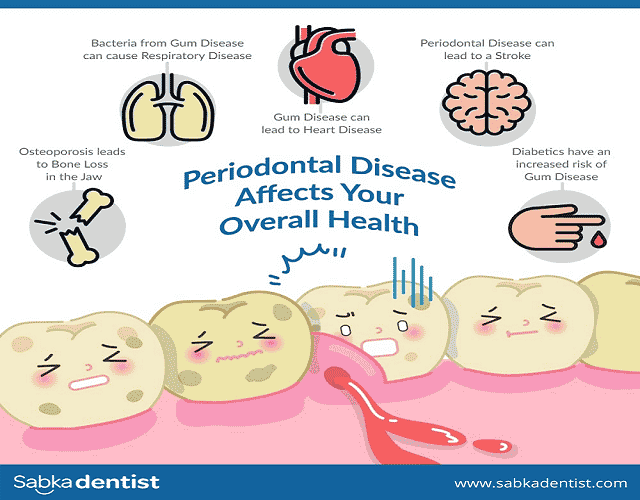
Scientists are concentrating on potential associations between gum disease and Atherosclerosis and coronary illness: Gum infection may build the danger of coronary disease, even though the degree of this association is vague. Gum ailment, likewise, is accepted to intensify existing coronary illness.
Stroke: Gum illness may build the danger of stroke that is brought about by blocked supply routes.
Diabetes: People with diabetes and periodontal infection might be bound to experience difficulty controlling their glucose than people with diabetes with healthy gums.
Respiratory sickness: Gum ailment may cause lung diseases and exacerbate existing lung conditions when microorganisms from the mouth move towards the lungs.
Healthy and active gums are light pink and are firm. They fit snuggly around teeth. Signs and manifestations of periodontitis symptoms can include:
- Swollen or puffy gums
- Brilliant red, shadowy red or purplish gums
- Gums that vibe delicate when contacted
- Gums that bleed more significantly.
- Gums that force away from your teeth (retreat), making your teeth look longer than typical
- New spaces creating between your teeth
- Discharge between your teeth and gums
- Awful breath
- Loose teeth
- Difficult biting
An adjustment in the manner your teeth fit together when you chew
Much of the time, periodontitis begins with plaque. It is a clingy layer made mostly out of microorganisms.
The plaque sits on your teeth when starches and sugars in food collaborate with microbes found in your mouth. Brushing your teeth twice a day and a daily floss can expel plaque, yet plaque re-gets back rapidly.
- Plaque can become solid under your gumline into tartar (mouth) if it remains on your teeth. Tartar is progressively hard to evacuate, and it’s loaded up with microorganisms. The more plaque and tartar stay on your teeth, the more damage they can do. You cannot dispose of tartar by brushing and flossing. You need proficient dental cleaning to evacuate it.
- Plaque can cause gum disease, the mildest type of periodontal infection. Gum disease is disturbance and aggravation of the piece of your gum around the base of your teeth (gingiva). Gum disease can be turned around with proficient periodontal treatment and great home oral well being.
- Continuous gum irritation can cause periodontitis in the long run, making periodontal pockets create between your gums and teeth that load up with plaque, tartar and microorganisms. In time, these periodontal pockets become further, loading up with more organisms. If not treated, these can profoundly damage the tissue and bone, and eventually, you may lose at least one teeth. Additionally, continuous constant aggravation can put a strain on your safe framework.
- Interminable periodontitis is the most widely recognized sort, influencing for the most part grown-ups. However, kids can be affected, as well. This sort is brought about by plaque development and includes moderate disintegration that may improve and deteriorate after some time; however, It aims pulverization in the bone and gum loss of teeth if not treated.
- Forcible periodontitis, for the most part, starts in youth or early adulthood and influences just a few individuals. It will, in general influence families and causes quick movement of bone and tooth misfortune if untreated.
- Necrotizing periodontal ailment is portrayed by the passing of gum tissue, tooth tendons, and supporting bone brought about by the absence of blood supply (rot), bringing about the severe disease. This sort, for the most part, happens in individuals with a stifled invulnerable framework, for example, from HIV disease, malignant growth treatment or different causes and hunger.
Treatment is planned for evacuating plaque and bacterial stores on your teeth and gums.
Oral cleanliness
Your dental consideration group will give you guidelines on the best way to lessen the number of microbes in your mouth, which includes keeping your teeth gum problems and help in gum disease treatment. Your dental specialist will offer you guidance on the best way to utilize toothbrushes and dental floss appropriately and may suggest other oral cleanliness items like a water pick or mouthwash.
Few tips for keeping your teeth in good condition:
- Brush your teeth two times every day with a fluoride toothpaste.
- Think about utilizing a rotating brush, which might be increasingly compelling.
- Floss daily to expel the chances of getting plaque.
- Visit your dental specialist, at least twice a year for an expert cleaning.
- Try not to smoke or bite tobacco.
Proficient cleanings

During an expert cleaning, your dental specialist will expel plaque development and tartar from your teeth and their underlying foundations, and afterwards clean your teeth and treat them with fluoride. Any periodontal pockets that have shaped could require deep cleaning to empower recovery. A profound cleaning strategy called scaling and root planning will assist with removing tartar and expel any unpleasant spots on the tooth root where microscopic organisms will generally assemble.
Anti-toxins
Your dental specialist will recommend anti-toxins to help with persistent gum diseases that haven’t reacted to cleanings. The anti-microbial may be as a mouthwash, gel, or an oral tablet.
Follow-up arrangements
Your dental specialist will need to catch up with you following half a month, and afterwards about each three to a half year after that to evaluate your advancement. If periodontal pockets are as yet present, they may suggest other treatment choices, similar to a medical procedure.
Medical procedure
If irritation endures in the mouth that is blocked off to brushing and flossing, your dental specialist may suggest a surgery called fold medical procedure to clean pores under your gums. Under anaesthesia, your gums are lifted away, and the underlying foundations of your teeth cleaned. Your gums are then sutured (sewed) once again into the right spot.
If you had any bone misfortune, a strategy known as bone uniting might be done simultaneously as fold medical procedure to recover the lost bone.
Albeit bacterial plaque development is the primary driver of periodontal sickness, a few different components, including various infections, meds and oral propensities, additionally can contribute.
These are factors that can build your danger of gum sickness or exacerbate it once the infection has set in.
- Heredity – Researchers accept up to 30% of the populace may have innate trouble to periodontal sickness. Having a genetic vulnerability, in any case, doesn’t mean gum infection is inescapable. Indeed, even individuals who are exceptionally inclined to the periodontal malady given their hereditary make-up can anticipate or control the ailment with significant oral consideration.
- Smoking and tobacco use – Smoking builds the danger of periodontal sickness, and the more one smokes, the higher the hazard. If a periodontal infection is present, smoking makes it increasingly severe. Smoking is the fundamental driver of periodontal ailment that is impervious to treatment. Smokers will, in general, gather more tartar on their teeth, create further periodontal pockets once they have gum illness and are probably going to lose bone as the infection advances. Not at all like numerous different variables that influence the strength of your gums, you have authority over this one. Stopping smoking can assume a significant job in managing the periodontal illness.
- Skewed or swarmed teeth, supports or bridgework – Anything that makes it progressively hard to brush or floss your teeth is probably going to upgrade plaque and tartar arrangement above and underneath the gum line, which builds your opportunity of creating gum treatment. Dental specialists and periodontists can show you the ideal approaches to clean your teeth, particularly in severe to-clean conditions. For instance, there are particular apparatuses and methods for stringing floss to clean around bridgework or slide underprops. Also, whenever stuffed or abnormal teeth are an issue, your dental specialist may prescribe orthodontics to fix your grin and give you a superior possibility of avoiding infection.
- Crushing, gritting or gripping of teeth – These propensities won’t cause periodontal sickness, yet they can prompt progressively extreme illness if irritation is as of now present. The over the top power applied on the teeth by these propensities seems to accelerate the breakdown of the periodontal tendon and bone. As a rule, patients can figure out how to stop this propensity basically by perceiving when it is occurring and afterwards unwinding. If these endeavors don’t work, your dental specialist or periodontist can make a custom watchman apparatus (at times called an occlusal monitor, night protect, mouth protect or nibble protect) that diminishes the weight of holding or crushing on the teeth.
- Stress – Stress can compound periodontal sickness and make it harder to treat. Fear debilitates your body’s insusceptible framework, which makes it harder for your body to fend off contamination, including periodontal infection.
- Fluctuating hormones – Whenever hormones vary in the body, changes can happen in the mouth. Pubescence and pregnancy can incidentally expand the hazard and seriousness of gum treatment, as can menopause.
- Prescriptions – Several types of medicines can cause dry mouth, or xerostomia, including antidepressants, diuretics and hypertension medications. Without the assurance of adequate measures of salivation, plaque is bound to frame. Different prescriptions may make the gums extend, which this way makes them bound to trap plaque. These prescriptions incorporate phenytoin (Dilantin and other brand names), used to control seizures, cyclosporine (Neoral, Sandimmune), used to smother the invulnerable framework. Other calcium channel blockers, used to treat heart arrhythmias or angina.
- Illnesses – Although the special instruments aren’t entirely comprehended, specific ailments increment vulnerability to periodontal sicknesses. For instance, individuals with diabetes are bound to get periodontitis than individuals without diabetes, and it’s probably going to be increasingly severe. Different ailments, for example, leukemia, provocative gut malady and HIV disease, additionally can build the hazard. Having one of these infections will take control of periodontal illness. Yet, a decent periodontist or dental specialist who knows about the new dangers and challenges ought to have the option to offer the sort of direction expected to keep up your periodontal wellbeing.
- Poor nourishment – Nutrition is significant broad wellbeing, including a working resistant framework and sound gums and mouth.
How can Sabka Dentist Help?
We offer effortless and customized dental treatment crosswise over Mumbai, Ahmedabad, Pune, Surat, and Bangalore.
Sabka Dentist can give the best dental consultation and satisfies the patient’s desires by providing them with the best periodontal treatment. The dental strategy utilized is innovative, that gives our patients a superior dental treatment experience. We spend significant time in all essential and day to day dental methodology like:
- Dental Check-up,
- Dental X-beams,
- Root Canal Treatment,
- Orthodontic Treatment (Braces),
- Teeth Scaling and Polishing,
- Dental Implants,
- Teeth Cleaning,
- Teeth Whitening and Bleaching,
- Dentures, and
- Overdentures.
With more than 500 dental specialists who are knowledgeable with dental practices and involvement with present-day dentistry, we allow them to deal with patient’s oral cleanliness at moderate costs. Our well-prepared dental specialists have confidence in giving quick and agony-free treatment to the patients keeping their oral wellbeing the top need. Just look for a periodontist near me and find us the top rated periodontal disease treatment center.
Here are some of the dental services that we offer:
- Consultation and Checkup: At every Sabka Dentist clinic, we give patients Consultation, X-Rays and dental checkup completely free. Our specialists prescribe you a complete a dental test like a clockwork to assist you with keeping up your oral cleanliness.
- Dental Veneers: The dental veneers are a slight layer of the tooth-like material, which is attached to the tooth surface with a negligible arrangement to improve style. The veneers can be utilized to change the shape, measure and colour of the teeth. Signs include stained teeth, broken teeth, distorted teeth, fluorosis, and so forth, the veneer is utilized. The surfaces look lovely and healthy and can keep going for over ten years. Our dental specialists offer the alternative of Ceramic and Composite Veneer.
- Periodontics: Teeth cleaning, scaling and cleaning: Our dental specialists in prescribe every patient to get cleaning/scaling done at regular intervals to keep up sound gums. It ought to be done to expel plaque and tartar from the tooth surface, which can generally harbour bacterial states.
- Endodontics: Root Canal Treatment is a consecutive treatment including expulsion of tainted mash from the carious tooth and it’s supplanting with gutta-percha material. The requirement for root canal treatment will be shown to the patient if required. At Sabka dentist, we have professional endodontic specialists to take care of your root canal.
- Oral Surgery: Our dental specialists will demonstrate extraction/evacuation of the tooth if the tooth is portable, or if there is some other explanation. We additionally have Oral Surgeons who are productive in performing other oral medical procedures like extraction of affected insight teeth, the healing process required for embed inclusion, and so forth.
- Pedodontics / Child Dentistry: Guardians regularly overlook issues in their youngsters teeth on account of the idea that they will fall away in any case. Milk teeth are significant because they are required for discourse, eating and to keep up space for permanent teeth. If milk teeth are stable, at that point the permanent teeth will in all probability be healthy and will come out in the right position. We have prepared Pediatric Dentists to treat your youngster at our dental facility.
At a dental visit, a dental specialist or dental hygienist will:
- Analyze your gums and note any indications of aggravation.
- Utilize a little ruler called a test to check for and measure any pockets around the teeth. In a sound mouth, the profundity of these pockets is as a rule somewhere in the range of 1 and 3 millimeters. This test for pocket profundity is normally effortless.
- Get some information about your clinical history to recognize conditions or hazard factors, (for example, smoking or diabetes) that may add to gum sickness.
The dental expert may likewise:
- Take an x-ray to see whether there is any bone misfortune.
- Allude you to a periodontist. Periodontists are specialists in the finding and treatment of periodontal and may furnish you with treatment alternatives that are not offered by your dental specialist.
Expert's Opinion
- Dr. Manan Dhulia Dental Director of Sabka dentist says “Periodontal disease is the leading cause of tooth loss in adults.”
- Dr. Preethi Nagarajan Dental Director of Sabka dentist says “Two most common periodontal diseases are: 1)Gingivitis: Inflammation of the gums at necks of teeth & 2) Periodontitis: Inflammation affecting the bone and tissues of teeth.”
- Dr. Reena Waghela Dental Director of Sabka dentist says “Periodontal disease is found to be associated with systemic conditions like diabetes, infective endocarditis, leukemia, etc.”
Frequently Asked Questions
How much does a dental checkup cost?
At Sabka Dentist, Dental checkup and X-ray consultation is free of cost.
How often should you get dental checkup?
Dental Checkup should be done every 6 months or biannually to detect any dental issues at an earlier stage and to maintain healthy teeth and gums.
What happens if you don’t get your teeth cleaned?
If your teeth are not cleaned regularly and if good oral hygiene is not maintained, plaque and calculus may buildup. Plaque tends to lower the pH and creates an acidic environment that may result in demineralization and tooth decay. Also, plaque and calculus buildup may result in inflammation of gums, bad breath, etc.
What does a (Periapical) Dental X-ray show?
Dental X-ray is valuable diagnostic tool that can help to confirm the final diagnosis of oral health condition. Radicular portion/ Root portion of tooth, which is not otherwise visible to the naked eye, can be displayed in an X-ray. Radiographs also help to determine the extent of decay, presence of cysts, bone loss etc. Congenitally missing or impacted teeth are often identified this way.
About Author

Dr. Priyanka graduated in 2008, obtained her BDS degree from the faculty of dentistry at the Maharashtra University of Health Sciences. Upon graduating, she was selected to complete a multi-disciplinary hospital residency at Government Dental College and Hospital, Mumbai. This residency provided her with advanced training in all the specialties of dentistry. Dr. Priyanka then moved to private practice, working as an associate dentist.
Dr. Priyanka has a diploma in Soft Tissue Lasers from IALD and fellowship in Implant & Esthetic Dentistry. Dr. Priyanka completed MBA in Hospital Management and Clinical Research. She has worked at Sabka Dentist since 2012 and is pleased to say that their advanced technology allows dentists like her to provide patients with painless, gentle dentistry and a pleasant experience.